First of all,
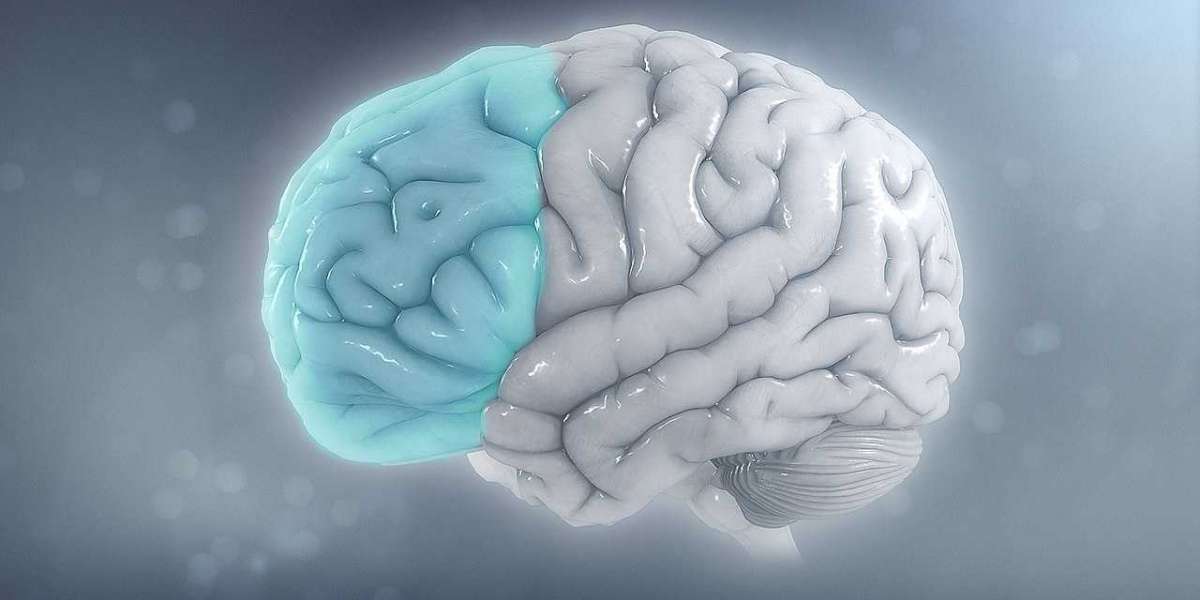
Millions of people worldwide are affected by the common and frequently incapacitating diseases known as headaches and migraines. These illnesses have different features even though they have some similar triggers. In this thorough investigation, we examine the various origins of headaches and migraines, look closely at their symptoms, and offer a wealth of information about practical treatment options.
Recognizing the Different Types of Headaches:
Tension-Type Headaches:
- Headaches of this type are the most prevalent and are characterized by a dull, continuous discomfort on both sides of the head.
- Causes: Tension-type headaches are frequently brought on by stress, tense muscles, bad posture, and sleep deprivation.
- Signs and symptoms: Sensitivity to light or noise, headache or neck tightness, and mild to moderate pain.
A migraine is a severe, throbbing headache that is frequently accompanied by other symptoms like nausea, vomiting, and sensitivity to stimuli.
- Causes: A number of variables, including genetics, hormone swings, triggers such as particular foods or environmental conditions, and abnormalities in neurotransmitters, may be involved.
- Severe pain, nausea, vomiting, aura (visual abnormalities), and increased light, sound, or scent sensitivity are among the symptoms.
Cluster Headaches:
- Overview: Usually affecting one side of the head, cluster headaches are unbearably severe headaches that come in clusters.
- Causes: Trigeminal nerve stimulation and anomalies in the hypothalamus are suggested causes, while the precise cause is unknown.
- Symptoms: Severe, searing, or penetrating pain; frequently accompanied by nasal congestion and red, watery eyes.
Sinus Headaches:
- Overview: Inflammation of the sinuses, or sinusitis, is linked to sinus headaches.
- Causes: Inflammation of the sinuses brought on by allergies, infections, or other conditions.
- Symptoms: Pressure and discomfort in the nose, cheeks, and forehead; this is frequently made worse by bending forward.
Typical Reasons for Migraines and Headaches:
Stress and Anxiety:
- Effect on Muscles: Tension in the shoulders and neck muscles can result from stress and anxiety, which can cause headaches that are similar to tension.
- Neurotransmitter Alterations: Stress increases may cause changes in neurotransmitter levels, which may aid in the development of migraines.
Hormonal Fluctuations:
- Menstrual Migraines: Certain people experience migraines as a result of hormonal fluctuations during the menstrual cycle.
- Birth Control tablets: The hormonal oscillations brought on by these tablets may affect the patterns of headaches.
Environmental Triggers:
- Weather Changes: Sudden variations in the weather, such as shifts in pressure, can set off migraine attacks.
- Overpowering Odors: People who are sensitive to the environment or certain smells or pollutants may get headaches.
Dietary factors:
- Caffeine Withdrawal: Because caffeine causes vasodilation and increased blood flow, abruptly stopping the drug might cause headaches.
- Food Triggers: For those who are prone, certain foods, such as cheese, chocolate, and processed meats, might cause migraines.
Sleep Disruptions:
- Sleep Deprivation: Insufficient sleep can exacerbate migraine susceptibility and cause tension-type headaches.
- Irregular Sleep Patterns: Scheduling sleep times inconsistently can throw off circadian cycles, which can lead to headaches.
muscular strain and Bad Posture:
- Neck and Shoulder Tension: Tension-type headaches are a result of both poor posture and chronic muscular strain in the neck and shoulders.
- Teeth grinding and jaw clenching: Temporomandibular joint (TMJ) strain brought on by bruxism can result in headaches.
Dehydration:
- Vasodilation and Reduced Blood Volume: Vasodilation brought on by dehydration can increase blood flow to the brain, which can result in headaches.
- Electrolyte Imbalance: When electrolyte balance is upset by dehydration, nerve function is impacted and migraines may result.
Genetic Predisposition:
- Family History: People who have a family history of migraines may be more likely to have these headaches due to genetic predisposition.
- Genetic Mutations: There is a link between certain genetic mutations and a higher migraine risk.
Methods of Headache and Migraine Treatment:
Lifestyle Adjustments:
- Stress Management: Techniques like progressive muscle relaxation, deep breathing, and mindfulness meditation can help relieve tension-type headaches.
- Regular Sleep: Headaches can be avoided by creating regular sleep schedules and emphasizing getting enough sleep.
Dietary Modifications:
- Identifying Triggers: Maintaining a headache journal to recognize and steer clear of possible dietary triggers for migraines.
- Hydration: Keeping up a sufficient fluid intake to avoid headaches brought on by dehydration.
Physical treatment:
- Posture Correction: This type of physical treatment addresses tense muscles and bad posture, which lowers the incidence of headaches with a tension-like feeling.
- Jaw exercises: Oral appliances and jaw exercises can help bruxism sufferers reduce stress and avoid headaches.
Medication Management:
- Pain medications: For mild to moderate headaches, over-the-counter pain medications like aspirin, ibuprofen, or acetaminophen are effective.
- Prescription Drugs: To reduce pain and stop episodes, triptans and other prescription drugs may be recommended for severe migraines.
Mind-Body Techniques:
- Biofeedback: By using biofeedback, one can effectively prevent tension-type headaches by learning to regulate physiological reactions to stress.
- Cognitive-Behavioral Therapy (CBT): Dealing with psychological issues and creating coping mechanisms to control anxiety and stress.
Acupuncture:
- in Traditional Chinese Medicine: By stimulating particular spots, acupuncture can enhance energy flow and lessen migraine frequency and intensity.
- Endorphin Release: Endorphins are a natural pain reliever that may be released by acupuncture.
Preventive medications include:
- Beta-Blockers: Propranolol, a beta-blocker, can help prevent migraines by lowering their frequency and intensity.
- Anticonvulsants: Topiramate is one medication that may be administered in specific circumstances to avoid migraines.
Nutritional Supplements:
- Magnesium: For those who are deficient in this element, taking supplements may help avoid migraines.
- Coenzyme Q10: According to certain research, taking a CoQ10 pill may help avoid migraines.
Counseling and Support:
- Psychoeducation: Educating people about headaches and migraines can give them the tools they need to take control of their problems.
- Support Groups: Attending therapy sessions or support groups can provide coping mechanisms and emotional support.
Surgical Interventions:
- Occipital Nerve Stimulation: This technique may be used to relieve pain in patients with chronic migraines that are unresponsive.
- Botox Injections: In order to paralyze specific muscles and lessen discomfort, botulinum toxin injections can be used to treat persistent migraines.
Issues and Matters to Take Into Account When Managing Headache and Migraine:
Individual Variability:
- Response to Treatments: Personalized management is necessary due to individual differences in treatment responses.
- Trial and error: Identifying the best course of action frequently entails a trial-and-error procedure.
Comorbid Conditions:
- Concurrent Health Issues: To treat several contributing causes, individuals with comorbid conditions may need an integrated strategy.
- Drug Interactions: It's important to carefully evaluate any possible interactions between headache treatments and other medical issues.
Lifestyle Adherence:
- Long-Term Commitment: For many non-pharmacological strategies to work as well as they should, long-term commitment and lifestyle adjustments are necessary.
- Behavioral Shifts: Depending on personal habits and preferences, adopting and sustaining a new lifestyle can present difficulties.
Multidisciplinary Care:
- Cooperation Among Specialists: Thorough headache management is ensured by efficient coordination and communication between medical professionals from different specializations.
- Holistic Approach: A holistic approach to headache and migraine treatment takes into account lifestyle, psychological, and physical issues.
In summary:
Effective management and cure of headaches and migraines require an understanding of their common causes. People can manage the complexity of these illnesses by recognizing their triggers, changing their lifestyle, and combining pharmaceutical and non-pharmacological interventions. When studies on headache and migraine mechanisms deepen, a multidisciplinary, patient-centered approach guarantees that each patient receives individualized care that is specific to their requirements and difficulties.